What is Tibial Interlocking Nail and How Does it Work?
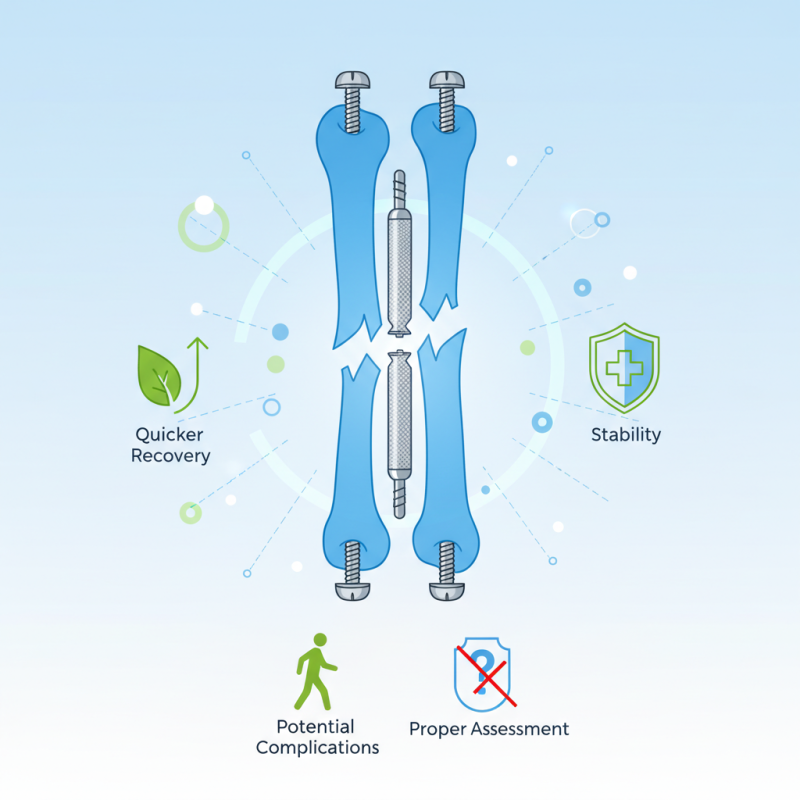
The Tibial Interlocking Nail is a vital tool in orthopedic surgery. It offers a way to stabilize fractures in the tibia, a key bone in the leg. The procedure involves inserting a metal rod through the tibia, enhancing healing and mobility. This technique is minimally invasive and can lead to quicker recovery times.
When a fracture occurs, using the Tibial Interlocking Nail can be a game changer. Surgeons place the nail through the bone and secure it with screws. This process aligns the bone properly, allowing it to heal correctly. Patients often experience less pain and can resume activities sooner than with traditional methods.
However, it is crucial to note that not all cases are perfect. Some patients may face complications like infection or improper alignment. Proper assessment is essential to avoid these issues. The benefits of the Tibial Interlocking Nail are clear, yet precautions and clear communication with patients are key to successful outcomes.
What is a Tibial Interlocking Nail?
A tibial interlocking nail is a sophisticated orthopedic device. It is used primarily to stabilize fractures in the tibia, the larger bone in the lower leg. This internal fixation method helps align the fractured bone ends to promote healing. Studies indicate that interlocking nails can lead to better outcomes, with complication rates dropping to around 5-10% in experienced hands.
The design of the tibial interlocking nail allows for the insertion of screws that lock into the nail. This mechanism provides enhanced stability. Reports reveal that this technique allows for early weight-bearing, which is crucial for a patient's recovery. Interestingly, not all patients experience the same level of benefit.
Variability in bone quality and fracture patterns can influence healing. In some cases, even with the best techniques, complications may occur. Issues such as infection or nail migration remind us that no procedure is free from risks. Research continues to evolve, but healthcare professionals must weigh these factors carefully.
Even with advanced technology, the human body can be unpredictable. It's vital to monitor patients closely and adjust treatment as necessary.
History and Development of Tibial Interlocking Nails
The tibial interlocking nail emerged from the need for effective fracture fixation in the tibia. The idea traces back to early orthopedic practices. Initial methods involved external fixation, which was often cumbersome and variable in effectiveness. With time, internal fixation gained prominence. The goal was to create a more stable and less invasive method for treating fractures.
In the late 20th century, the design of the tibial interlocking nail evolved significantly. Surgeons sought to improve upon earlier intramedullary nails. The incorporation of locking mechanisms allowed for enhanced stability. This marked a pivotal shift in orthopedic treatment. Yet, early designs were not without flaws. Complications sometimes arose, including infection and malalignment. Continuous feedback from surgical teams helped refine the technique.
Even today, there are challenges to address. Some patients report discomfort post-surgery. Also, not every fracture type is suitable for this method. Surgeons must carefully assess each case. Research continues to push the boundaries of this technique. The evolution of tibial interlocking nails reflects both progress and the need for ongoing improvement.
Indications for Using Tibial Interlocking Nails
Tibial interlocking nails are essential for stabilizing complex fractures in the tibia. These medical devices are especially indicated for the treatment of unstable fractures, such as those resulting from high-energy trauma. According to a study published in the Journal of Orthopaedics, nearly 40% of tibial fractures require surgical intervention due to their unstable nature. Interlocking nails provide a robust method for achieving internal fixation by locking within the bone, promoting proper alignment and healing.
Many surgeons opt for tibial interlocking nails in cases of open fractures and significant bone loss. The interlocking mechanism helps prevent rotational and axial instability during the healing process. A report by the American Academy of Orthopaedic Surgeons notes that these nails can reduce recovery time by up to 30% compared to traditional casting methods. However, surgical complications, such as infection or malunion, can occur, leading to patient dissatisfaction and additional surgeries.
Tips: Always discuss with your surgeon about the risks and benefits of using tibial interlocking nails. Consider getting a second opinion if your case is complex. Choosing the right approach can significantly impact your recovery journey. Remember, each case is unique, and what works for one patient might not be suitable for another.
What is Tibial Interlocking Nail and How Does it Work? - Indications for Using Tibial Interlocking Nails
| Indication | Description | Advantages | Considerations |
|---|---|---|---|
| Femoral Fractures | Used for stabilizing specific types of femoral fractures. | Allows for early mobilization, minimal soft tissue disruption. | Requires careful surgical technique; risk of infection. |
| Bilateral Fractures | Facilitates treatment of both limbs when fractures occur. | Enhanced stability; can be done with minimal surgical approach. | Increased complexity; potential for longer recovery. |
| Non-union Fractures | Provides stabilization in cases where bone healing has stalled. | Improves chances of successful healing; maintains limb function. | Requires assessment of underlying causes of non-union. |
| Pediatric Applications | Used in certain pediatric fracture cases. | Minimally invasive; preserves growth plates. | Requires careful monitoring for growth-related issues. |
Surgical Procedure for Tibial Interlocking Nail Insertion
The surgical procedure for tibial interlocking nail insertion is precise and methodical. Surgeons start by positioning the patient correctly, often under general or spinal anesthesia. Once the site is prepped, they make a small incision near the knee or ankle. The goal is to create a pathway for the interlocking nail to fit snugly within the tibia.
Using fluoroscopy, surgeons guide the nail through the bone. This real-time imaging helps ensure accurate placement. After insertion, they use locking screws to secure the nail in place. Careful attention is required; it's crucial to avoid damaging surrounding tissues. Additionally, some patients may experience complications, like infection or malalignment, which need to be addressed during recovery.
Post-surgery, patients are usually encouraged to begin rehabilitation. This might include limited weight-bearing and physical therapy. While the nail provides stability, time and commitment are essential for complete recovery. Each step of the process requires reflection and adaptation. The journey varies for everyone, emphasizing the need for personalized care plans. Each patient's experience informs better practices for future procedures.
Postoperative Care and Rehabilitation with Tibial Interlocking Nails
Postoperative care is essential after tibial interlocking nail surgery. Patients should monitor their incision sites. Watch for signs of infection like redness or swelling. Keeping the area clean is vital for healing.
Physical therapy plays a significant role in recovery. Gentle exercises can help regain mobility. Start with simple movements, focusing on knee and ankle flexibility. Over time, you'll progress to strength-building exercises.
Tips: Rest is crucial, but too much can lead to stiffness. Listen to your body. If something feels off, it’s okay to reach out for advice. Also, eating a balanced diet can support bone healing. Stay hydrated and consider supplementing with vitamins. This can enhance your recovery experience.
